Modifiable vs Non-Modifiable Risk Factors for Heart Disease : A Complete Guide
Heart disease is a silent plague responsible for more deaths globally than any other illness. Whether you’re young or old, heart health should come first. The good news? While some risk factors are beyond your control, many are not. Understanding the difference between modifiable and non-modifiable risk factors for heart disease can help you take meaningful steps toward prevention.
This guide breaks down both types of risk factors, with a focus on modifiable risk factors for heart disease, the ones you can change to safeguard your heart.
 Understanding Risk Factors for heart disease.
Understanding Risk Factors for heart disease.
A risk factor is anything that increases the likelihood of developing a disease. When it comes to heart disease. When it comes to heart disease, these risk factors fall into two categories:
- Modifiable risk factors for heart disease – these are lifestyle and behavioral choices you can change to reduce your risk.
- Non- modifiable risk factors – these are traits you cannot change, such as your age, sex, or family history
The key to prevention lies in managing the modifiable risk factors, while staying informed and proactive about the non-modifiable ones.
 Modifiable Risk Factors for Heart Disease (Lifestyle & Preventable Causes)
Modifiable Risk Factors for Heart Disease (Lifestyle & Preventable Causes)
The good news is that many risk factors for heart disease are completely within your control. These modifiable factors are closely tied to your lifestyle choices and habits. Addressing them can dramatically reduce your risk of developing cardiovascular issues.
1. High Blood pressure (Hypertension)
Uncontrolled high blood pressure strains your heart, damage arteries, and is one of the most significant contributors to heart disease.
| Control Tip: Reduce salt intake, manage stress, and follow a regular exercise routine. Medications may also be necessary for some individuals.
2. High cholesterol and triglycerides levels
Elevated LDL (“bad”) cholesterol and triglycerides can lad to plaque buildup in arteries, narrowing them and increasing the risk of heart attack or stroke.
| Heart-Smart Move: Eat more fiber, eliminate trans fats, increase omega-3s, and stay physically active.
3. Smoking and tobacco use
Cigarette smoke damages the lining of your arteries, increases blood pressure, and reduces oxygen in your blood, all major contributors to heart disease.
| Did you know? Quitting smoking lower your risk of heart disease within just 1 year of stopping. 4. Physical Inactivity
A sedentary lifestyle weakens your heart and promotes other risk factors like obesity and diabetes. Regular physical activity improves circulation, reduces blood pressure, and strengthens the heart.
| Goal: Aim for at least 150 minutes of moderate aerobic activity per week, such as brisk walking, swimming, or cycling.
4. Unhealthy Diet:
Diets high in saturated fats, processed foods, added sugars, and sodium can trigger inflammation, weigh gain, and cholesterol imbalances.
| Try this: Follow a heart- healthy eating pattern like the mediterranean or DASH diet rich in vegetables, fruits, lean proteins, and whole grains.
5. Overweight and obesity
Excess weight especially around the abdomen can increase your risk of high blood pressure, insulin resistance, and high cholesterol.
| Important Note: Even a 5 – 10% reduction in body weight can lead to major improvements in cardiovascular health.
6. Excessive Alcohol consumption:
Too much alcohol can raise blood pressure, lead to weight gain, and contribute to irregular heart rhythms like atrial fibrillation.
| Recommended Limits: No more than one drink per day for women, and two for men or avoid alcohol altogether.
7. Chronic stress and poor mental health
Long term stress can lead to unhealthy copying behaviors (e.g., overeating, smoking) and may raise blood pressure and heart rate.
| Copying tools: Practice mindfulness, deep breathing therapy, or physical activity to manage stress effectively.
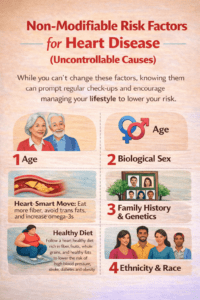 Non- Modifiable Risk factors for heart disease (Uncontrollable causes )
Non- Modifiable Risk factors for heart disease (Uncontrollable causes )
While you can’t change these factors, awareness allows for early intervention and prevention. If you fall into one or more of these categories, it’s even more important to manage you modifiable risks.
1. Age
Your risk for heart disease increases with age. Most heart attacks occur in people aged 65 or older.
| Why it matters: Aging causes natural wear and tear on blood vessels and the heart muscle
2. Biological Sex
Men tend to develop heart disease earlier than women, but women;s risk increases after menopause and may even surpass that of men.
| Takeaway: Women’s symptoms can be subtler, fatigue, nausea, and shortness of breath are common signs of heart trouble.
3. Family History and genetics
If a close relative (parent or sibling) had heart disease at an early age (before 55 for men and 65 for women), your own risk may be higher.
| Genetic awareness: While you can’t change your genes, early screening and proactive lifestyle changes can minimize their impact.
4. Ethnicity and race
Certain ethnic backgrounds are at greater risk. For Example:
- South Asians often face early onset of heart disease.
- African americans are more prone to high blood pressure and stroke.
- Hispanic and native american populations may have higher rates of diabetes and obesity | Cultural Health tip: Customize prevention strategies to fit your cultural dietary patterns and health behaviors.
Taking Charge: Prevention starts with what you can control
Understanding the difference between modifiable and non-modifiable risk factors for heart disease gives you a roadmap to action. Even if you carry certain non- changeable risks, addressing the modifiable risk factors for heart disease can dramatically lower your change of illness.
Here’s how to start:
- Eat a diet low in saturated fats and added sugars
- Stay active throughout the week
- Stop smoking completely
- Manage stress through mindfulness and breathing techniques
- Monitor your blood pressure, blood sugar and cholesterol regularly
- Know your family history and discuss it with your doctor
