Your Blood Clotting Speaks Volumes About Your Liver Health

Your annual health check-up can reveal more than just your cholesterol or sugar levels; it can offer a glimpse into how well your liver is functioning. One of the key markers that often appears on your report is INR and liver health, or International Normalized Ratio.
At first glance, it might just look like another lab number. But behind this figure lies a powerful clue about your blood’s ability to clot and, more importantly, the health of your liver.
What Is INR and Why It Matters INR and liver health
INR measures how long it takes your blood to form a clot compared to an average (normal) value. Think of it as a “clotting score” the higher the number, the longer your blood takes to clot.
For a healthy adult, the normal INR range is between 0.8 and 1.2. An INR of 1.0 means your blood clots in about the same time as the population average. Each increase of 0.1 means your blood is “thinner” and takes slightly longer to clot.
While INR is widely used to monitor patients on blood thinners like warfarin, it’s equally vital for those with liver disease. That’s because the liver makes most of the proteins needed for blood clotting. When it’s damaged, these proteins decrease and your INR rises.
Simply put, a higher INR can signal impaired liver function, even if you’re not taking any anticoagulant medications.
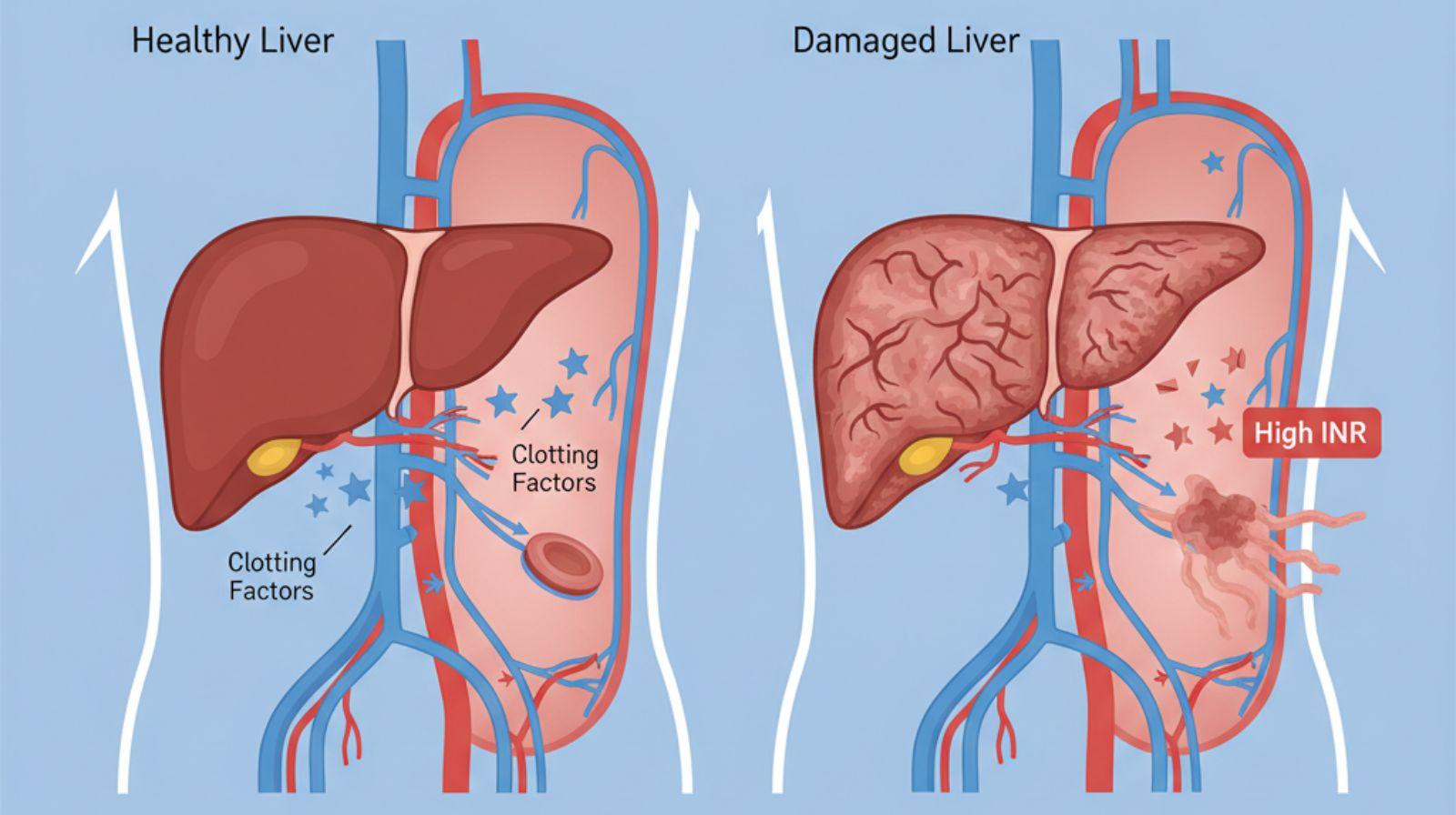
How Your Liver Affects INR
Your liver is your body’s multitasking hero — it metabolizes nutrients, stores energy, filters toxins, and plays a key role in blood clotting.
When your liver is healthy, it produces enough clotting factors — special proteins that help your blood form clots quickly when you’re injured. But in conditions like hepatitis, fatty liver disease, cirrhosis, or alcohol-related damage, your liver’s ability to make these proteins drops.
This reduction leads to a prolonged clotting time, reflected as a higher INR. Doctors pay close attention to this value because it helps them understand how efficiently your liver is performing.
A rising INR can be an early warning sign of liver dysfunction even before more obvious symptoms like jaundice, fatigue, or swelling appear.
Normal INR Ranges and What They Mean
| INR Range | What It Means | Possible Implication |
| 0.8 – 1.2 | Normal range for healthy individuals | Normal clotting |
| 1.3 – 1.5 | Slightly elevated | May indicate mild liver dysfunction or vitamin K deficiency |
| 1.6 – 2.0 | Moderately high | Liver disease likely impacting clotting protein synthesis |
| >2.0 | Significantly elevated | Severe liver impairment or increased bleeding risk |
The Prothrombin Time (PT) test measured in seconds forms the base for calculating INR. INR standardizes PT results, ensuring your values are comparable across different labs.
When your INR climbs above 1.5 without being on any blood-thinning medication, it can often suggest that your liver’s synthetic function is declining. Doctors use this information to assess both the severity and progression of liver disease.
High INR: Risks and What to Watch For
A high INR generally means your blood takes longer to clot. This can increase your risk of bleeding, especially during injuries, dental procedures, or surgeries.
However, liver disease can complicate this picture. Some patients with high INR don’t bleed easily; in fact, they might even face a higher risk of clot formation a condition known as rebalanced hemostasis.
In advanced liver disease, both clotting and anti-clotting factors drop, creating a delicate balance. That’s why INR alone doesn’t always predict bleeding risk but remains an essential part of monitoring overall liver health.
When to Be Concerned
You should contact your healthcare provider if you notice:
- Easy bruising or frequent nosebleeds
- Bleeding gums
- Blood in stool or urine
- Persistent fatigue, yellowing of eyes or skin (jaundice)
- Swelling of feet or abdomen
Before any surgery or procedure, your doctor may adjust medications, administer vitamin K, or recommend plasma transfusions to stabilize INR levels and reduce bleeding risk.
Factors That Influence INR (Vitamin K, Medications, etc.)
Several factors can affect INR, not just liver health. Understanding these helps you interpret your results better:
1. Vitamin K
Vitamin K is crucial for making clotting factors. A deficiency — common in liver disease and people with poor diet or absorption issues — can increase INR.
2. Medications
Certain medications, especially antibiotics, antifungals, or blood thinners like warfarin, can raise INR levels. Always inform your doctor about all medications and supplements you’re taking.
3. Diet
Sudden changes in dietary vitamin K intake (from foods like spinach, kale, or broccoli) can alter INR readings, though this is more relevant for patients on anticoagulants.
4. Chronic Illnesses
Kidney disease, heart failure, and chronic infections can indirectly affect liver function and, consequently, INR levels.
5. Alcohol and Toxins
Excessive alcohol use directly damages liver cells, decreasing clotting protein synthesis and pushing INR higher.
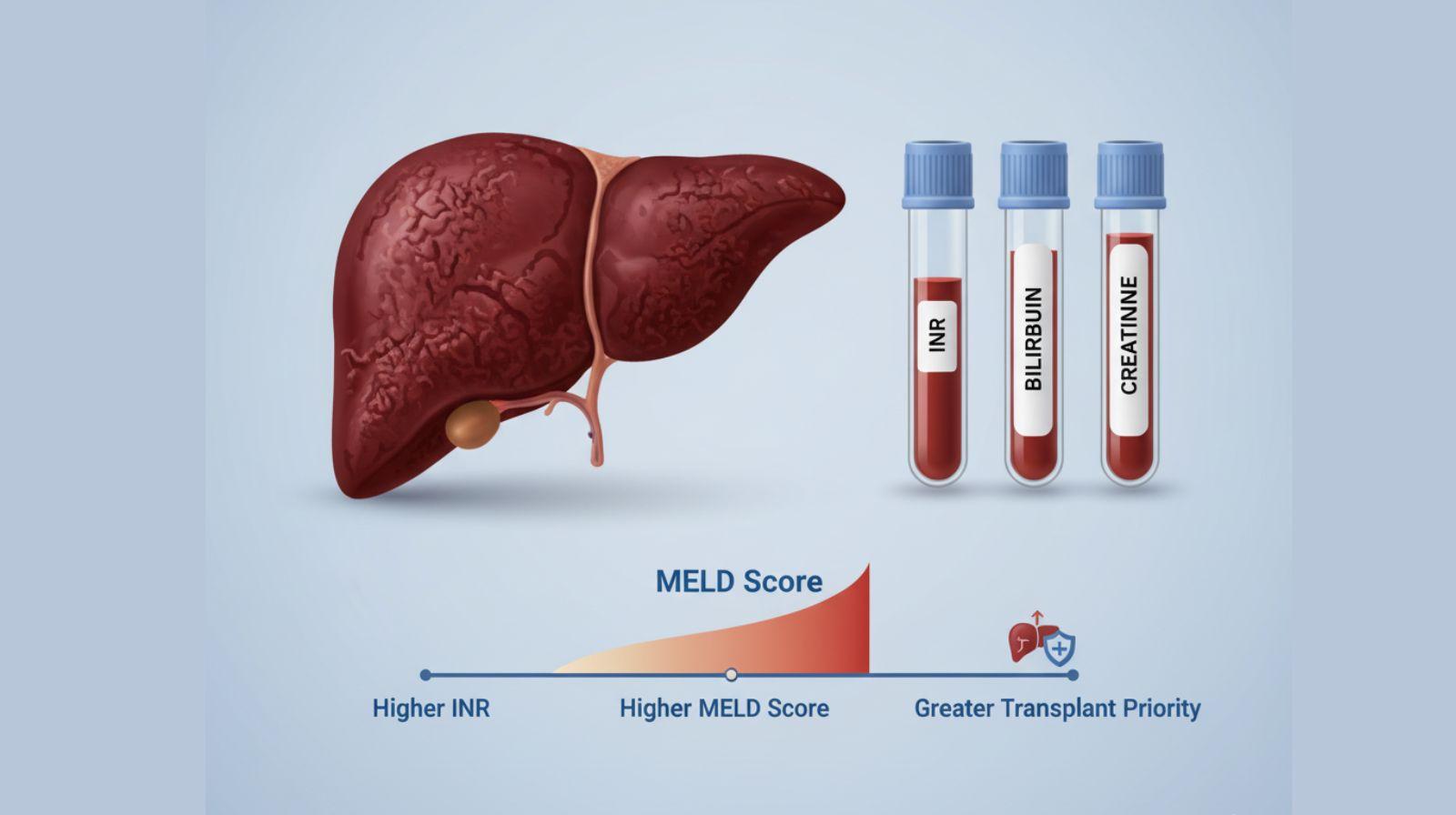
INR in Liver Disease Monitoring (MELD Score and Transplant Priority)
In patients with chronic or advanced liver disease, INR is not just a diagnostic tool it’s a prognostic marker.
Doctors use it as part of the MELD (Model for End-Stage Liver Disease) score, which predicts how severe liver disease is and helps prioritize patients for liver transplantation.
The MELD score is calculated using:
- INR
- Bilirubin
- Creatinine
A higher INR contributes to a higher MELD score, signaling worse liver function and greater urgency for transplant.
Studies have shown that patients with INR above 2.0 have a higher risk of complications and mortality. Regular monitoring helps doctors adjust treatments, manage risks, and make timely decisions about advanced care or transplant evaluation.
FAQs About INR and Liver Health
-
Can I lower my INR through diet or supplements?
Not directly. When INR elevation is due to liver dysfunction, dietary changes usually won’t normalize it. However, vitamin K supplementation may help in specific cases, but only under medical guidance.
-
Will High INR increase my risk of bleeding?
Not necessarily. In liver disease, high INR simply reflects your liver’s reduced ability to make clotting proteins. Doctors interpret INR in context with your overall clinical picture. You are not at the risk of bleeding in daily life.
-
What’s the risk if my INR is too high?
A very high INR (especially above 2.0) increases the risk of spontaneous bleeding, particularly from the gums, nose, or gastrointestinal tract. It can also signal a critical decline in liver function.
-
Why is INR part of the MELD score?
Because it reflects how well the liver produces clotting proteins. A higher INR usually means a more severely damaged liver, helping doctors prioritize patients who need urgent transplant care.
-
How often should INR be checked if I have liver disease?
The frequency depends on your condition’s severity. Mild cases may require testing every few months, while advanced liver disease might need weekly or monthly monitoring.
Takeaway: Your INR Is More Than Just a Number
Your INR isn’t just a lab value — it’s a window into your liver’s health. Whether you’re managing fatty liver, hepatitis, or cirrhosis, tracking INR helps your doctor monitor how well your liver is functioning and how to prevent complications.
If your INR is rising, don’t panic — it’s your body’s way of signaling that it needs attention. Regular follow-ups, healthy lifestyle choices, and open communication with your healthcare team can go a long way in protecting your liver and your life.
References
References:
1.https://medlineplus.gov/liverdiseases.html
- https://www.hepatitis.va.gov/hcv/patient/diagnosis/labtests-INR.asp
- https://www.sciencedirect.com/science/article/pii/S1538783622129739
- Harrison MF. The Misunderstood Coagulopathy of Liver Disease: A Review for the Acute Setting. West J Emerg Med. 2018 Sep;19(5):863-871. doi: 10.5811/westjem.2018.7.37893. Epub 2018 Aug 8. PMID: 30202500; PMCID: PMC6123093.
- https://www.jacc.org/doi/10.1016/j.jacc.2018.03.023
- https://emcrit.org/ibcc/cirrhosis/